Stay Sex Safe: Preparing for Post Lockdown Relationships
As the UK embarks on its roadmap to lockdown relaxation, the world looks ahead to a return to ‘normality’. And while there are many positives for us to look forward to, a new report from the analysts at Medicine Direct has revealed potential challenges in sexual health that will face us in the weeks and months to come.
Through an analysis of nearly 4 million Google searches from March to July 2020, it is shown that the number of people looking for emergency contraception rose by 41% between the start and end of lockdown one, while searches for STD tests rose 51% in the same period.
With this analysis comes a stark warning for the UK as we approach the end of lockdown three; stay sex safe.
What does ‘Stay Sex Safe’ mean?
The Stay Sex Safe campaign intends to educate the nation on the necessity of a cautious return to sexual relationships.
Much like the three word phrases that drove behaviours through lockdown, its intention is to plant the seeds for sexually educated behaviours across the country and to encourage safer sex practices as we find ourselves back together in a post-lockdown world.
The following is a guide to staying sex safe; as with all medical advice, please reach out to medical professionals if you have any queries or personal concerns.
Stay Sex Safe: Birth Control
Birth control is the term used to describe any method of reducing the potential of a pregnancy occurring as a result of sexual intercourse. There are various options available to you; speak to your doctor if you’re unsure.
Condoms
Condoms are worn on the penis during sexual intercourse and they reduce the chances of pregnancy by containing the ejaculate to lessen the likelihood of fertilisation.
The Pill
The Pill is the term commonly used to refer to the various forms of pill taken to prevent the release of eggs (ovulation) and thicken the lining at the neck of the womb to make it more difficult for sperm to enter.
IUD / Coil
A hormonal IUD is a T shaped device which is inserted into the vagina and which releases copper that thickens the lining of the cervix and makes it very difficult for sperm to survive.
Implant
The contraceptive implant is placed into the upper arm under the skin by your doctor or nurse. It releases progesterone into your bloodstream which prevents pregnancy.
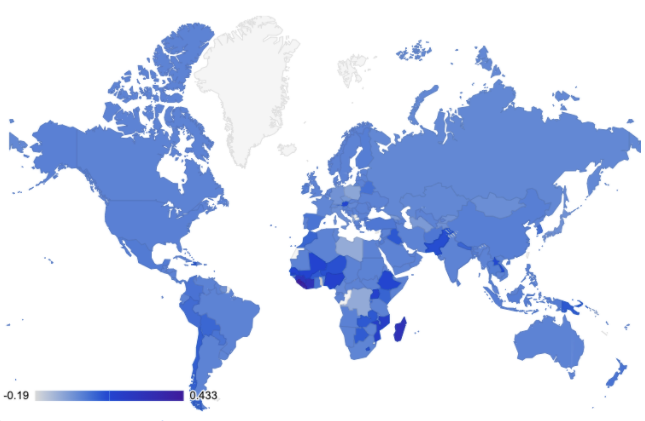
Birth control around the world
Use of birth control differs around the world in line with trends, costs and personal preferences. The map below uses data sourced from the United Nations World Contraceptive Reports from 2016 to 2020 and shows the change in use of all contraceptives, where the darker the blue, the greater the increase in contraceptive use in that country:
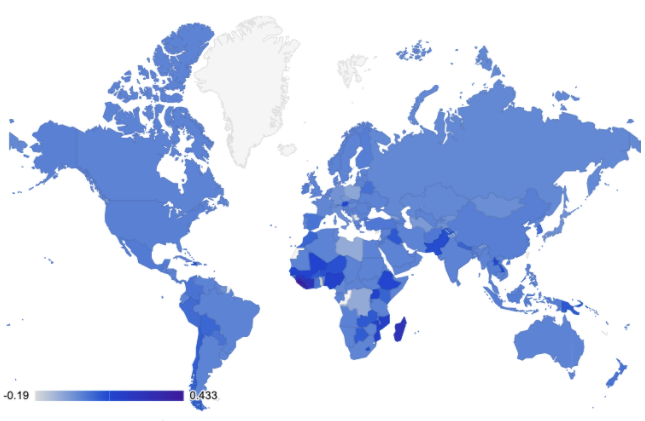
Source: United Nations World Contraceptive Reports 2016 - 2020
The countries with the greatest increase in contraceptive use are shown below, with the UK, Ireland and USA added:
Country |
5 Year Change |
|
Sierra Leone |
43.28% |
|
Liberia |
36.58% |
|
Côte d'Ivoire |
27.03% |
|
Madagascar |
26.57% |
|
Guinea |
24.48% |
|
Mozambique |
16.81% |
|
Nigeria |
14.20% |
|
Uganda |
13.74% |
|
Mali |
12.22% |
|
Senegal |
12.08% |
|
Ireland |
1.36% |
|
United Kingdom |
0.00% |
|
United States of America |
0.50% |
The countries with the greatest percentage growth in use of the various contraceptives are shown in the table below:
IUD |
Pill |
Male Condom |
Emergency Contraception |
|
|
1 |
Papua New Guinea |
Poland |
China |
Ireland |
|
2 |
Mozambique |
Finland |
Niger |
Nigeria |
|
3 |
Ireland |
Côte d'Ivoire |
South Africa |
Brazil |
|
4 |
Guinea |
Madagascar |
Germany |
Iran (Islamic Republic of) |
|
5 |
New Zealand |
Lao People's Democratic Republic |
Poland |
Germany |
|
6 |
Burkina Faso |
Democratic People's Republic of Korea |
Tajikistan |
Ethiopia |
|
7 |
Mali |
Sierra Leone |
Belarus |
Ghana |
|
8 |
Ethiopia |
Italy |
Iraq |
Austria |
|
9 |
Madagascar |
Niger |
New Zealand |
Estonia |
|
10 |
Benin |
Spain |
Côte d'Ivoire |
Stay Sex Safe: Emergency Contraception
Emergency contraception is the term used to describe contraceptives used after sex, most commonly the morning after pill (or ‘plan B’). It is typically used if sex has occured without protection or where the protection has failed, such as a split condom.
Emergency Contraception (the morning after pill) has to be taken within 72 hours of sex in order to be effective and is most effective when taken sooner rather than later.
An IUD can also be used as emergency contraception if fitted within 5 days of unprotected sex.
Emergency contraception is only applicable to birth control and does not provide protection against sexually transmitted disease (STDs) after the fact.
The cost of emergency contraception
The cost of emergency contraception differs around the world and is monitored by the European Consortium for Emergency Contraception. The table below shows the cost of emergency contraception in the form of the Levonorgestrel-only EC pill.
The UK has the highest cost of emergency contraception in Europe based on an analysis of all 46 countries monitored by the EC for EC:
Country |
Cost (Euros) |
|
United Kingdom |
42 |
|
Ireland |
40.47 |
|
Slovakia |
22 |
|
Croatia |
21.4 |
|
Czech Republic |
21 |
|
Hungary |
19.3 |
|
Finland |
18.87 |
|
Switzerland |
17.5 |
|
Malta |
17 |
|
Germany |
16 |
Source: European Consortium for Emergency Contraception
The costs above represent average purchase costs in Euros. Here in the UK, we can obtain emergency contraception free of charge through the NHS but where visiting the GP is difficult or an individual does not feel comfortable in seeking GP support, emergency contraception can also be purchased through high street pharmacies and online pharmacies like Medicine Direct.
Emergency contraception during Covid-19
In an average month, nearly 126,000 people search for terms relating to and including ‘emergency contraception’. This number increased by 26% at the end of lockdown one across all related phrases and specifically by 41% for the exact term ‘emergency contraception’.
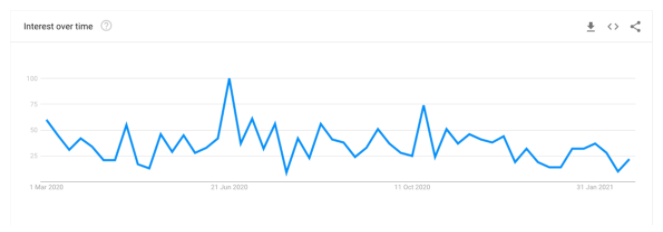
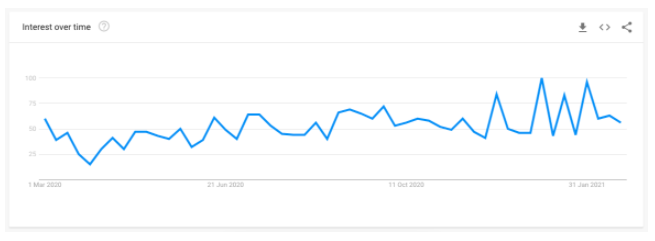
The chart above shows the points where searches for ‘emergency contraception’ spiked following the end of each lockdown, with the last week in June 2020 having the highest peak of the year. There was also a spike just before the November lockdown when it was announced on the 31st October.
While access to the morning after pill can be free of charge in the UK, this is only possible with a prescription. In most cases, waiting for a GP appointment is not possible for many women who require the morning after pill. With the average wait to get a GP appointment now exceeding 15 days, this would essentially make the morning after pill ineffective as it needs to be taken with 5 days of unprotected sex. It is also advised that emergency contraception is most effective the sooner it is taken after sex.
The two main morning after pills are:
- ellaOne - This should be taken within 120 hours (5 days after sex)
- Levonelle 1500 - This should be taken within 72 hours of sex
According to data from GP Online, 4 in 10 Brits avoid visiting the GP during Covid-19. Google search data shows that an average of 8,100 people every month search for ‘emergency contraception; if 40% of those choose to purchase EC rather than go to a doctor, this would equate to a cost of €136,080, or £117,522 every month based on the average cost of EC.
The UK’s lockdown relaxation roadmap is due to last until July 2021; assuming 4 in 10 people continue to avoid the GP until then, this could mean a cost of £470,088 in emergency contraception over the next 4 months - another reason for the Stay Sex Safe message.
Stay Sex Safe: Sexually Transmitted Disease (STDs)
Sexually transmitted diseases (STDs - or STIs, meaning sexually transmitted infections) are contracted through unprotected sexual contact, including penetration and oral sex. It is important to use a condom for any form of sexual contact unless all participants have been checked and cleared of any STDs.
Over the course of 2020, STDs such as chlamydia were at a 5 year low, as shown by our recent UK STI Check report. However, like contraception, the number of searches for STD checks increased dramatically following each lockdown relaxation - leading to predictions of similar as we progress through 2021.
According to our analysis of Google data, the number of people looking for STD related terms increased by 22% when comparing the average number of monthly searches to those made in July 2020. Searches for the specific term “STD testing” rose by 34% and for “STD testing near me” by 53%.
Searches for “STD test” have subsequently spiked further over the festive period when lockdown regulations were relaxed, suggesting we as a nation are becoming more conscious of our sexual health as we move toward lockdown’s end.
Our recent analysis also showed that 53% of Brits have never had an STD test - meaning that STDs such as chlamydia which have no physical symptoms could be spreading without our knowledge, raising concerns for the months ahead.
Understanding STD symptoms
The symptoms of STDs / STIs are fairly easy to spot where they exist and should be acted upon quickly. Common symptoms include:
- Unusual discharge
- Pain when urinating
- Unusual and painful vaginal bleeding (most women mistakenly look for specific period pain treatment or generic pain relief medicine to help with period pain instead of checking for an underlying condition/possible STD infection)
- Lumps or growths around the genitals or anus
- Unusual genital itching
- Blisters, sores or a rash around genitals or anus
If you experience any of these symptoms, you should speak to a qualified medical professional for advice.
You can view our complete guide to STD symptoms here.
Common STDs
Common STDs include:
Chlamydia
This is one of the most common STDs in the UK and is most prevalent amongst younger people. It is recommended that you be checked or use a chlamydia test kit annually or every time you change partner as the symptoms often go undetected.
Gonorrhoea
The bacteria that cause gonorrhea are found in the discharge from the penis or vagina and is passed through unprotected sexual contact or the sharing of sex toys that have not been cleaned or covered with a condom. It is characterised by symptoms of unusual discharge. Gonnorhoea is also now getting more and more difficult to treat within the UK due to the emergency of "Super Gonorrhoea" and antibiotic resistance. As a result, gonorrhoea is treated by combining Cefixime and Azithromycin.
Genital warts
Genital warts are painless lumps around the vagina, penis or anus, characterised by itching, bleeding or a change to the normal flow of urine.
Pubic lice
Pubic lice are sometimes called ‘crabs’ and are tiny insects that live in pubic hair, spread through close sexual contact. Pubic lice can also live in underarm, chest or facial hair but not on scalp hair.
If you have any concerns about STDs, it’s important to get checked out by a qualified professional.
STDs around the UK
In our annual UK STI health check, we asked Brits to tell us how often they were STI tested.
UK regional variation
In exploring global approaches to birth control, we have also analysed Google search data throughout the UK to understand regional variation, too.
To do this, the largest five cities in each region have been selected and data pulled from Google’s own platform to compare the number of searches pre and post lockdown in 2020. The regional changes are shown below:
Search Query |
South of England |
Midlands |
North of England |
Scotland |
Wales |
|
emergency contraception |
3.50% |
7.14% |
16.22% |
0.00% |
25.00% |
|
morning after pill |
19.57% |
9.49% |
9.79% |
15.08% |
33.33% |
|
nexplanon |
34.19% |
67.74% |
82.86% |
53.13% |
16.67% |
|
combination pill |
0.85% |
6.25% |
0.00% |
10.00% |
0.00% |
|
intrauterine device |
-2.84% |
-18.27% |
-9.46% |
-7.59% |
-26.09% |
|
birth control |
2.26% |
12.24% |
2.22% |
-6.90% |
0.00% |
|
std testing |
22.54% |
0.89% |
18.92% |
22.22% |
14.29% |
|
std testing near me |
21.54% |
7.69% |
30.00% |
20.00% |
|
|
sexual health clinic near me |
48.54% |
19.80% |
41.44% |
46.15% |
57.14% |
|
std check |
18.82% |
0.00% |
18.52% |
-16.67% |
0.00% |
How can we Stay Sex Safe post-lockdown?
Staying sex safe will be an essential consideration as our society starts to move toward reintegration. While we’re all understandably excited at the prospect of being together again, previous lockdown data shows us that we’re at greater risk of lowering our sexual barriers and therefore opening ourselves up to potential issues such as unwanted pregnancy or STDs.
The following tips are designed to provide guidance to everyone of a sexually active persuasion during this time but, as with all the advice you find on the internet, should always be supplemented by advice from your own doctor/medical professional if you’re at all unsure.
- Get an STD test
Some STDs have clear symptoms, while others can lie undetected due to a lack of clearly identifiable symptoms. Either way, the STDs have the potential to cause much bigger issues if left untreated and we should be conscious of our own potential to spread such infections if we are not treated, too.
Via an online consultation, you can purchase chlamydia tests for home use. You can also speak to your local sexual health clinic who will advise you over the telephone and invite you in if the need exists - find your local sexual health clinic with this handy guide from the NHS.
- Use a condom
Condoms are 98% effective at preventing the spread of STDs like chlamydia and gonorrhea, so wearing them for any sexual contact, including oral, is a good way to protect yourself and your sexual partner(s).
Condoms cannot protect you against STDs such as herpes or genital warts though, as these are spread through skin to skin contact - hence the importance of being STD checked.
- Consider your options for birth control
Birth control is facilitated through the use of a condom but, as shown in this guide, there are other options available to you which can be used as well. Considering your options is a personal choice and will be dependent on your future plans and preferences.
If you’re unsure at all, you can reach out to a medical practitioner for personalised advice.
- Keep an open conversation about sexual wellbeing
2020 has taught us a lot and one of the greatest lessons we hope will persevere post-lockdown is that of the importance of open and honest conversations.
This relates to mental health most prominently as we have all tried to learn to be more open in our conversations around mental wellbeing and support. But it is true also for our sexual wellbeing; we need to be willing to talk openly about our sexual health and to be confident in discussing sexual topics with our sexual partners, our confidantes and our medical health practitioners.